The healthcare system continues to face a number of challenges, from rising costs to provider shortages, but one of the most impactful—and often overlooked—areas for improvement is the quality of communication between physicians and their patients. Studies have repeatedly shown that when communication is clear, empathetic, and consistent, patient satisfaction rises significantly. More importantly, so do patient outcomes. Effective communication isn’t simply a soft skill; it’s a foundational element of high-quality healthcare.
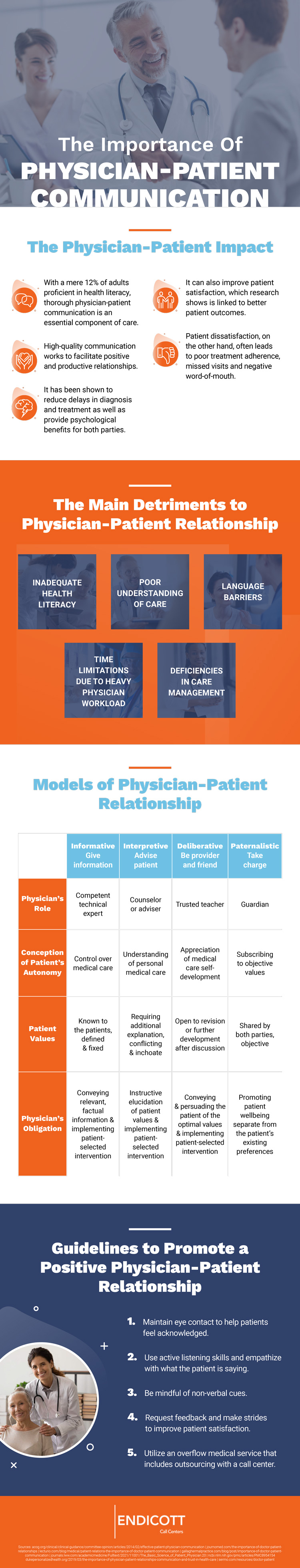
Unfortunately, several barriers exist that prevent optimal communication from taking place in clinical settings. Chief among them is the lack of health literacy among patients. According to the U.S. Department of Health and Human Services, only about 12% of adults are considered proficient in health literacy. This means the vast majority of patients may struggle to understand important information about their conditions, medications, and treatment plans. Whether due to complex medical jargon, cultural differences, or cognitive limitations, the result is the same: confusion, miscommunication, and poor adherence to medical instructions.
Physicians play a crucial role in bridging this gap. Building trust from the first encounter is essential. Simple gestures—like offering a warm greeting, maintaining eye contact, and exhibiting genuine concern—can help set a welcoming tone. Moreover, the use of plain language rather than medical terminology enables clearer understanding. Active listening, where the physician reflects back what the patient is saying or asks clarifying questions, further ensures mutual understanding. Equally important is non-verbal communication, including body posture, facial expressions, and tone of voice, all of which can either reinforce or undermine the spoken message.
One strategy to enhance clarity is the “teach-back” method, where patients are asked to explain the instructions they’ve received in their own words. This not only confirms comprehension but also highlights areas that may require further clarification. Physicians should also be attentive to cues that patients may not be following the conversation—such as nodding without asking questions—or hesitating to speak. Providing written materials in easy-to-understand language, supplemented by visuals when possible, can reinforce verbal instructions and offer patients a reference point once they leave the office.
Beyond the individual physician-patient relationship, systemic and organizational improvements are also necessary. Many healthcare environments are strained by understaffing, overbooked schedules, and administrative burdens that limit the time doctors can spend with patients. Addressing these limitations could include reevaluating scheduling systems to allow for longer appointments where needed, or integrating support services such as health coaches or patient navigators to reinforce key messages. In fact, some healthcare networks have begun leveraging the services of a dispatch call center to ensure follow-up care instructions are reiterated, questions are answered post-visit, and continuity of care is maintained even after a patient leaves the facility. This kind of centralized communication support can make a substantial difference in long-term outcomes and patient adherence.
Encouraging regular visits, especially for patients with chronic conditions or those recovering from surgeries or hospitalizations, is another critical piece of the puzzle. Continuity of care allows physicians to monitor progress, adjust treatment as needed, and address patient concerns before they escalate. Additionally, implementing feedback loops—such as patient satisfaction surveys or digital communication tools—can offer insights into what’s working and where gaps still exist.
Effective physician-patient communication doesn’t happen by accident. It requires training, intentional effort, and a culture that prioritizes compassion alongside clinical excellence. When providers commit to clear, respectful, and empathetic communication, they do more than inform—they empower. And empowered patients are more likely to engage in their care, follow medical advice, and ultimately, experience better health outcomes.
For a deeper dive into strategies for strengthening physician-patient communication and its impact on health, please consult the accompanying resource.